You know that phenomenon when you notice a pattern somewhere and you can’t believe you hadn’t seen it before, and suddenly you start seeing it everywhere? It’s even more eye-opening when there was something you thought was a little ‘off,’ but you couldn’t quite figure it out and then, once you do, you realize it’s a cancer. Hindsight and all that.
I volunteered to be part of a task force for my local school district in 2018. Our job was to dig deeply in to the “highly capable” program and come up with ways to make it less elite (less white, less geared toward rich families, less racist). We spent months looking at data, examining the history of the program, the laws surrounding it, the myriad ways the district had tried to identify and serve kids with extraordinary academic prowess over the years, and how other districts were doing it. It was no secret that our system was deeply flawed from beginning to end.
We weren’t the first group of folks to ever attempt this here. Indeed, there had been a similar task force just a few years earlier that had done the same thing – volunteering hundreds of hours of their time to come up with recommendations they put forth to the district, many of which got a head nod and a sad, “we wish that were possible” before retiring to the packet of information to be passed along to the next task force – us.
We were a fairly diverse group of parents, educators, and community members – cutting across racial and ethnic lines, but not really across socioeconomic ones. I mean, if you have to be able to offer your labor for free for 18 months and show up at prescribed times in a central location, it’s not exactly feasible for many folks, is it? But we did our best to try and bring voices in to the room that may not have been represented.
I think it was around month 12 that I finally figured it out. And now I can’t unsee it. And I also can’t not notice it everywhere I look.
We were never going to be able to make radical, substantive change to this system because no matter what we did, the system had a way of continuing to center itself.
Supposedly, the public school system was created to benefit kids and society (well, mostly society if we’re being honest). Over time, we started thinking that the benefit to kids would work itself out if we just threw a little money and a bunch of rules at it. We kept adding layers and layers of bureaucracy (standardized testing, mandatory minimum days/hours of instruction, core class requirements, etc. etc.) without ever looking at the impact it truly had on society or the kids. And even if we recognized that some of those things were detrimental or not really serving the kids, the system had invested so much time and money in to setting up the scaffolding for those things, we weren’t about to abandon them. When we went in to that task force work, it was with the goal of increasing equity, but that has to do with the kids, what’s good for them, and the system kept saying, “how can we do that?” or “how can we pay for that?”
It’s the same with our “health care” system. We don’t center the patient – we center the system. Asking how we can afford it, or wringing our hands as we think about the logistics of dismantling the private insurance system and the administrative bureaucracy fed by it is centering the system. The system has taken over and become our driving, bedrock force in every decision. We consider the needs of the individuals only within the context of the system’s needs being met, not the other way around. We bend over backwards to try and find solutions (add layers of bureaucracy) to protect the system. That’s why Joe Biden wants to have a private insurance option and just expand Obamacare. Not for the good of the collective, the good of the individual human beings, but so we don’t disrupt the system.
That is why women and people of color and folks with disabilities and those along the gender and sexuality spectrum are the progressives – because they have historically not ever been served well by the systems we put in to place and they are willing to center the collective, the human beings. But the white men who are served really well by capitalism, indeed, who have their identities tied up so deeply with capitalism and colonialism, feel threatened.
So many of the things we take for granted – 40-hour work week, retiring at 65, the stock market as the measure of the economy – those are things that were set up to benefit the system. If we don’t question them, when we want to make things better for the people who aren’t served well by the system, we just add little appendages here and there. Overtime pay, retirement jobs at Walmart as greeters, no-fee online investing opportunities. WE ARE CENTERING THE SYSTEM.
But here’s the thing: this time in history right now is showing us that we can live outside the system, that we can find ways to center people.
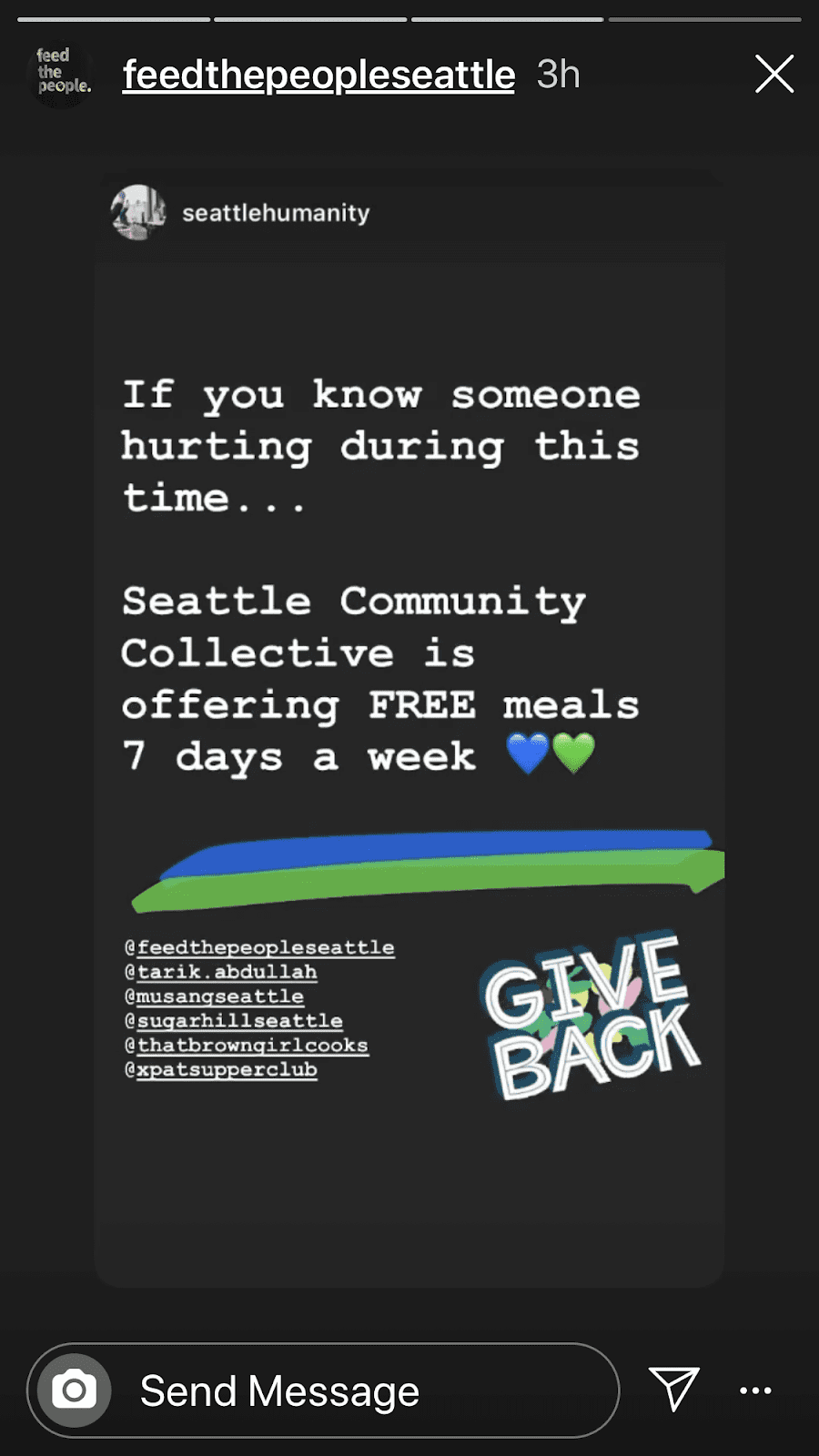
Do you know how vulnerable people are getting fed right now? Not through systems – in SPITE of systems. There are collectives springing up all over the place to feed people who need it, neighbors offering to shop for other neighbors and deliver groceries to their doors, donations of gift cards to folks in need, people sending money through Venmo to people they’ve never met before. People centering people.
Do you know how people are going to survive not paying their rent? Not because of systems. The systems aren’t responding quickly enough – there are too many layers to cut through. If we suspend rent payments, we have to suspend mortgages for the landlords and if we do that, we have to bail out the banks who hold those mortgages and then people will be mad that we bailed out the banks, etc. etc. But local folks are banding together to form coalitions that are demanding that renters not be evicted and that rent be suspended – without penalty or interest – for now. There are millions of dollars in grant money flowing to artists and small businesses impacted by this because of individual people who centered the collective good.
Small farmers who were de-centered in favor of the system are banding together to find ways to get food to folks who want it. And in many cases, it’s working. Because we are centering people, not systems.
The huge hospitals that are cutting pay for healthcare workers because their clinics have all but shut down for elective visits? They’re centering the system. They are saying “we can’t pay for this” instead of saying “we will do what it takes to make sure that everyone is taken care of.”
The politicians who refuse to order shelter-in-place rules? They’re centering the system. They are saying “having people out buying and selling things in my community is more important than the health and well-being of the community.”
That pathetic stimulus package check you may or may not get? Centering the system. Even it doesn’t address everyone – college students who live on their own but are still claimed as dependents on their parents’ taxes get no check, social security beneficiaries whose threshold income is too low to file a tax return get no check.
The thing is, the system will tell you that it is working for the greater good, for the collective. But it isn’t. The system is working for itself. Anytime you hear “what will that cost?” or “we can’t logistically manage that,” you are witnessing a system centering itself. These systems are crumbling for a reason right now and that is because they rely on people to make them work, whether they serve the people or not. The system will try to coerce a certain number of people to stick with them by any means possible (overtime pay, threats of job loss, appealing to the needs of others), but make no mistake, your needs are not paramount.
One evening toward the end of our task force work, I walked out in to the dark parking lot alongside a teacher who works with students with special needs. We talked about our frustration and our hope that we hadn’t just been wasting hundreds of hours of our own time to come up with strong, bodacious recommendations that would simply be cast aside by the Superintendent. I talked to her about my theory of systems centering themselves and she got teary and it was then that I realized she was the inflection point and I felt overwhelmed for her. In a system that centers itself, if you are a teacher or a health care worker who truly centers the person you’re supposed to be serving, you are caught in a vise. In order to keep your job and do the work you do that you believe is so vital, you have to bow to the system. But in order to serve the children or the patients who come to you in the way they deserve to be served, you have to eschew all of the principles the system wants you to embrace – you have to be creative, find workarounds, often use your own resources to go above and beyond. The system is hurting us all if we truly want to center people and the collective good, not only the individuals being served, but those who are exhausting themselves and their resources to be the conduit between the systems and the collective.
It’s time for another way. May we use the next several weeks to dismantle the systems that center themselves. May we find the strength and courage to answer the question “how can we pay for that?” by saying “it doesn’t matter – we have to do what is right.” May we remember that if we value each other, we can look to the underground groups that are springing up to help each other outside the system and learn from them. This truly is the Matrix and we’re seeing the glitches.


